What Is a Bicornuate Uterus and How Does It Affect Fertility?
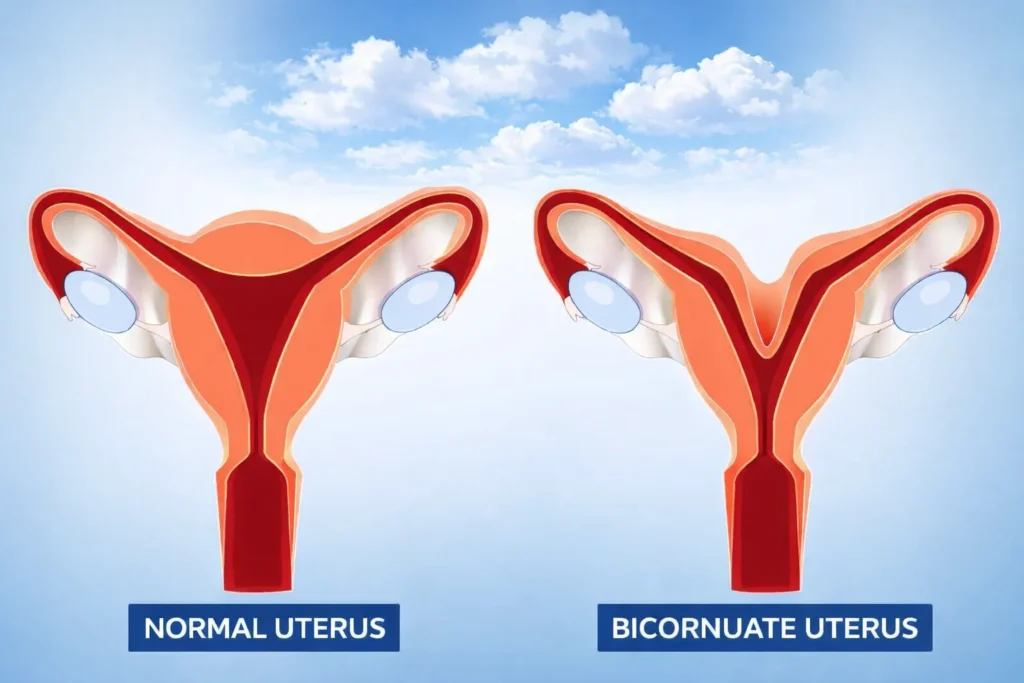
A bicornuate uterus (uterus bicornis) is a congenital Müllerian duct anomaly classified by the American Society for Reproductive Medicine (ASRM) as a fusion defect of the uterus. It is characterized by a heart-shaped uterine cavity with two upper horns, caused by incomplete fusion of the Müllerian ducts during embryonic development.
The condition is considered rare, affecting approximately 0.4% of women in the general population.
For many women, the diagnosis comes unexpectedly. It may be discovered incidentally during a routine pelvic ultrasound or after months—or even years—of searching for answers following recurrent miscarriages or preterm birth. This moment is often accompanied by fear, uncertainty, and concerns about future fertility and pregnancy outcomes.
Understanding what a bicornuate uterus is and how it affects fertility helps women replace fear with clarity and make informed medical decisions.
Anatomy of a Uterus
Normal Uterine Development
During early fetal life, the uterus forms from two paired structures called Müllerian ducts. In normal development:
- The ducts fuse completely in the midline
- The central wall dissolves
- A single, pear-shaped uterine cavity forms
What Happens in a Bicornuate Uterus
In a bicornuate uterus:
- Fusion of the Müllerian ducts is incomplete
- The upper portion of the uterus remains divided
- A deep indentation (cleft) forms at the fundus
- Two uterine horns develop instead of one cavity
This structural difference is present from birth and is not influenced by lifestyle, diet, sexual activity, or hormonal changes later in life.
Bicornuate Uterus Explained
A bicornuate uterus is one of several congenital uterine anomalies. The degree of separation determines clinical risk.
Types of Bicornuate Uterus
Partial Bicornuate Uterus
- Mild indentation at the fundus
- Two cavities partially separated
- Lower risk of pregnancy complications
Complete Bicornuate Uterus
- Deep division extending toward the cervix
- Significantly altered uterine shape
- Higher risk of miscarriage, preterm birth, and malpresentation
The greater the separation, the more limited the space available for a growing pregnancy.
Symptoms and Causes
Symptoms of a Bicornuate Uterus
Many women remain asymptomatic. When symptoms occur, they are usually related to pregnancy:
- Recurrent first- or second-trimester miscarriage
- Preterm labor
- Breech or transverse fetal position
- Pelvic pain or pressure
- Painful menstruation (in some cases)
The abnormal uterine shape restricts space, which can interfere with fetal growth and positioning.
Bicornuate Uterus Causes
A bicornuate uterus develops before birth due to:
- Incomplete Müllerian duct fusion
- Genetic and developmental factors
- Rare intrauterine environmental influences
Important myth clarification:
Lifestyle habits, exercise, sexual activity, infections, or diet do not cause a bicornuate uterus.
Bicornuate Uterus Sonography and Diagnosis
What the Diagnostic Process Feels Like
- 2D ultrasound: Initial screening, painless, 10–15 minutes
- 3D ultrasound: Gold standard; provides precise visualization
- Hysterosalpingography (HSG): Contrast X-ray; may cause brief cramping
- MRI: Used when diagnosis remains uncertain
Why 3D Ultrasound Is the Gold Standard
3D ultrasound allows doctors to visualize the external contour of the uterine fundus, which is critical for differentiating a bicornuate uterus from a septate uterus—a distinction that directly affects treatment decisions.
Is a Double Uterus the Same as a Bicornuate Uterus?
No.
| Condition | Key Difference |
|---|---|
| Bicornuate uterus | One cervix, two upper cavities |
| Uterus didelphys (double uterus) | Two separate uteri and two cervices |
Correct diagnosis prevents unnecessary surgery.
Bicornuate Uterus Pregnancy and Fertility
Can I Get Pregnant If I Have a Bicornuate Uterus?
Yes. Fertility itself is usually normal.
However, pregnancy outcomes require closer monitoring.
Pregnancy Risks (With Data)
- First-trimester miscarriage: 25–30%
- General population: 10–15%
- Preterm birth risk: Increased
- Malpresentation: Common
Despite these risks, over 70–80% of women achieve a live birth with modern obstetric care.
Representative Clinical Case
A typical clinical scenario involves a woman diagnosed after recurrent pregnancy loss. With early identification, serial ultrasounds, cervical length monitoring, and planned delivery, she carries a pregnancy to term and delivers a healthy infant—often via cesarean section.
This reflects real-world outcomes seen in specialized obstetric care.
Complications Associated With a Bicornuate Uterus
- Cervical insufficiency
- Preterm premature rupture of membranes (PPROM)
- Placental abruption
- Preterm labor
Not all women experience complications, but high-risk prenatal care significantly improves outcomes.
Management and Treatment
How Is It Treated?
Most women do not require treatment.
Non-Surgical Management
- Bi-weekly cervical length measurements (weeks 16–24)
- Serial fetal growth scans
- Progesterone therapy in selected cases
Surgical Treatment
- Strassmann metroplasty
- Considered only in rare cases of repeated second-trimester loss despite optimal care
Routine surgery is not recommended.
Labor and Delivery Considerations
- Increased likelihood of cesarean delivery
- Breech presentation is common
- Early labor monitoring required
Many women deliver safely with planned obstetric care.
Outlook / Prognosis
With modern diagnostics and prenatal monitoring:
- Live birth rates exceed 70–80%
- Emotional outcomes improve with education
- Long-term gynecologic health is usually unaffected
Differential Diagnosis: Why Accurate Diagnosis Matters
| Condition | Key Feature | Treatment |
|---|---|---|
| Septate uterus | Internal septum | Often surgical |
| Arcuate uterus | Mild indentation | No treatment |
| Bicornuate uterus | External fundal cleft | Monitoring |
FAQs: Bicornuate Uterus
Can a bicornuate uterus cause infertility?
No. Fertility is usually unaffected.
Is pregnancy always high risk?
Not always, but closer monitoring is recommended.
Does everyone need surgery?
No. Surgery is rare.
Does it affect menopause or general health?
No significant long-term effects outside pregnancy.
Conclusion for Patients
A diagnosis of bicornuate uterus can feel frightening—especially when fertility or pregnancy is involved. Medical evidence shows that most women conceive naturally and deliver healthy babies, especially when the condition is recognized early and managed appropriately.
A bicornuate uterus is a structural difference, not a failure of the body. With informed care, clear guidance, and supportive monitoring, the outlook is overwhelmingly positive.
A Note from Lotus Femcare
At Lotus Femcare, we understand that learning about a condition like a bicornuate uterus can bring up many questions, emotions, and uncertainties—especially when fertility and pregnancy are involved. Every woman’s body and journey are unique, and uterine differences do not define your ability to experience a healthy pregnancy or a fulfilling reproductive life.
You are not alone in this journey. With awareness, early diagnosis, and appropriate medical support, many women with a bicornuate uterus go on to have positive pregnancy outcomes and healthy lives.